Epistaxis in the Elderly: Causes, Risks & First Response

When a nosebleed strikes an older adult, it can feel more alarming than it really is. A trickle of blood may seem minor, but when it’s coming from someone with delicate skin, blood-thinning medications, or multiple health concerns, even a small bleed can cause big worry.
Nosebleeds — or epistaxis, to use the medical term — are fairly common in the elderly, but they’re not always well understood. Sometimes they’re harmless, sometimes they’re a warning sign. The key is knowing when to treat it at home, when to call for help, and how to reduce the risk in the first place.
Why Do Nosebleeds Happen More Often in Older Adults?
Nosebleeds in later life might feel random, but they’re usually not. They’re the kind of small health hiccups that show up when a few common factors mix — like dry air, thinning skin, or medications doing their job a little too well. And while they’re usually not serious, they can still be alarming, especially the first few times.
So, what’s really going on when Gran or Pop gets a sudden nosebleed while watching telly?
1. Delicate Noses and Fragile Blood Vessels
With age, the skin (including the inside of the nose) becomes thinner and more fragile — kind of like your favourite old tea towel that’s just one wash away from fraying. The blood vessels sitting just under that delicate surface are more likely to break, especially after a good nose-blow or a rogue sneeze. According to Healthdirect Australia, this is one of the top reasons nosebleeds happen more frequently in older adults.
2. Dry Air + Ageing Skin = Trouble
Whether it’s winter heaters, dry weather, or constant air con, the nasal passages can dry out fast. A dry nose is a cranky nose — it can crack, crust, and bleed at the drop of a hat. This is super common in aged care settings or homes with heating, where humidity levels drop and noses suffer.
3. Medications That Thin the Blood
Many older adults are on blood thinners like aspirin or warfarin to keep their hearts healthy. The downside? They can also make small bleeds trickier to stop. As pointed out by Griswold Home Care, these medications can turn a mild nosebleed into something more dramatic — especially if it catches you off guard.
4. High Blood Pressure
Not everyone feels their high blood pressure, but your nose might. When blood pressure is high, it puts extra force behind even a small bleed, making it gushier than usual and a bit harder to control. According to University Hospitals, this can be a key reason why some nosebleeds feel like they’re never going to stop — even though they do.
5. Nose-Picking or Blowing (Yes, Still)
Look, we’re not here to point fingers — but sometimes, a quick scratch inside the nostril or a forceful tissue blow can be the culprit. Even the mildest cold can make noses more sensitive, and it doesn’t take much to start a bleed when the nasal lining is already dry and delicate.
6. Underlying Health Conditions
More rarely, conditions like liver disease, blood disorders, or even nasal growths (yep, they happen) can lead to frequent or hard-to-control bleeds. If nosebleeds are showing up more often than reruns on daytime TV, it’s a good idea to check in with a GP and rule out anything serious.
Why Nosebleeds Can Be Tricky in Aged Care
On paper, managing a nosebleed sounds simple enough — sit them upright, lean forward, pinch the nose. But when you're caring for an older adult at home or in an aged care setting, the reality can look very different.
Here’s why:
1. Limited Mobility = Limited Reactions
Older adults may not be able to move quickly or reposition themselves without help. Something as straightforward as sitting upright and leaning forward — the recommended first response for nosebleeds, according to Better Health Channel — may require a carer’s assistance or mechanical aid. This delay can lead to longer bleeding times and a greater mess (not to mention distress for the person involved).
2. Cognitive Impairments Complicate Care
For seniors with dementia or cognitive decline, staying calm during a nosebleed may not be possible. As Healthdirect Australia explains, applying first aid requires the person to remain still and breathe through their mouth. In practice, a confused or frightened senior may panic, swat at their face, or even resist help — making the situation harder for everyone.
3. Medication Conflicts Are Real
Blood thinners like aspirin or warfarin are common among older adults. While they’re vital for managing stroke or heart disease risk, they also mean that even a small bleed can take longer to stop. As Hartford HealthCare Senior Services notes, this makes nosebleeds both more frequent and more severe in elderly populations — especially those on anticoagulants or anti-inflammatory medications.
4. Delayed Reporting = Bigger Messes
Many older adults don’t feel a nosebleed starting until it’s already well underway. Add in hearing or vision impairments, and some bleeds may go unnoticed or unreported until there’s visible blood on clothing or furniture. This not only complicates cleanup but also adds emotional stress for both carers and the person affected.
5. Understaffed or Overstretched Environments
In group aged care settings, where one staff member may be responsible for multiple residents, an immediate first aid response isn’t always guaranteed. A single nosebleed can draw attention away from others, especially if there’s a risk of falling or confusion. This makes clear protocols and accessible first aid products essential for aged care teams.
First Aid Refresher for Nosebleeds in Aged Care (With a Few Pro Tips)
When nosebleeds strike, especially in aged care settings, staying calm and prepared makes all the difference. Here’s a practical, reassuring guide for carers — with a few product tools to make your response safer, cleaner, and more effective.
1. Position Them Properly: Upright and Forward
Help the person sit upright with their head tilted slightly forward — this helps reduce blood pressure in the nasal vessels and prevents blood from running down the throat, which can cause nausea or choking. Avoid tilting their head back.
Carer Tip: If the person is frail, recovering from surgery, or has trouble sitting up on their own, use a supportive recliner.
Try This: Royale Medical Chadwick Leather Lift Chair

This lift chair offers gentle reclining and upright support at the push of a button. It’s ideal for managing first aid incidents with minimal fuss — and adds daily comfort for clients with mobility challenges.
2. Pinch the Nose — Gently, With Gloves
Wearing medical gloves, use your fingers to pinch the soft part of the nose just below the bony bridge. Hold steady pressure for at least 10 minutes. Don’t stop to check early — it resets the clotting clock.
Try This: SafeGuard+ Blue Nitrile Examination Gloves

These powder-free gloves offer superior dexterity and hygiene during any first aid task. Comfortable, ambidextrous, and latex-free — they’re a must-have for home carers, aged care workers, and clinics alike.
3. Skip the Tissues — Use Clinical Nasal Packing if Needed
If the bleed continues or is coming from deeper inside the nose, avoid stuffing tissues or gauze — they can worsen the bleeding or cause trauma. Instead, reach for a medical-grade nasal device designed for safe tamponade.
Try This: Rapid Rhino Inflatable Tamponade Device
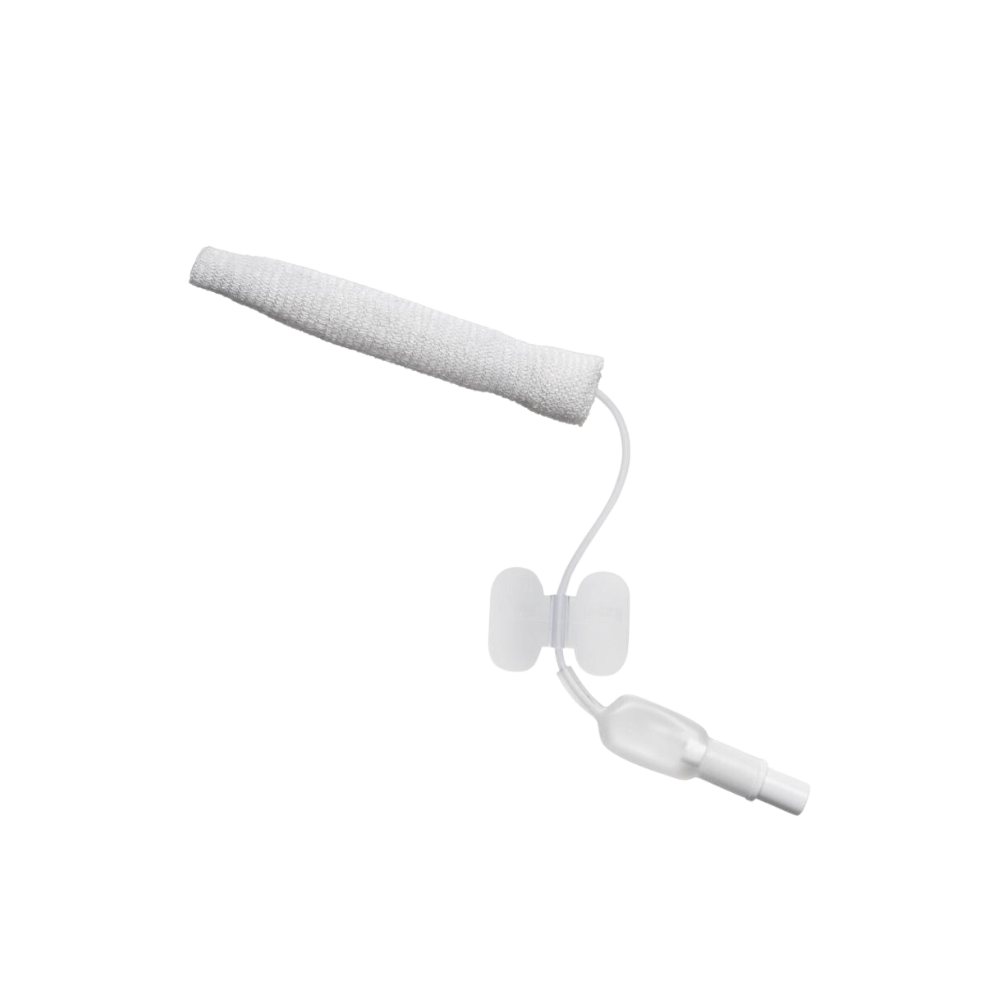
Specially developed to manage epistaxis gently and effectively, the Rapid Rhino uses controlled pressure and cooling to stop bleeding with less trauma. It’s particularly helpful for older adults with fragile nasal tissues or blood thinners.
4. Comfort and Reassurance Matter
Apply a cool compress to the back of the neck or forehead — not to stop bleeding, but to help calm and comfort the person. Reassure them with gentle words and stay close. A calm carer can ease the entire experience.
5. When to Call for Help
Most nosebleeds resolve with pressure and positioning. But it’s time to seek medical help if:
- The bleeding doesn’t stop after 20 minutes
- There’s dizziness, fainting, or rapid heartbeat
- The person is on blood thinners
- There are frequent or recurring nosebleeds
- Blood is running into the throat or being coughed up
As Healthdirect, Better Health Victoria, and Hartford Healthcare all affirm, severe or persistent nosebleeds in the elderly warrant medical assessment — especially when paired with frailty, falls risk, or underlying conditions.
How to Prevent Nosebleeds in Older Adults: Practical Everyday Tips
When it comes to nosebleeds in aged care, prevention really is better than panic. While an occasional bleed can be harmless, frequent or spontaneous episodes may point to an avoidable trigger. Here’s how carers, family members, and aged care staff can help reduce the risk — one small habit at a time.
1. Keep the Nasal Passages Moist
Dry nasal membranes are one of the most common causes of nosebleeds in older adults, especially during winter or in heated indoor environments. As Cleveland Clinic explains, fragile capillaries in the nose can crack and bleed when the lining dries out.
Prevention Tip: Use a saline nasal spray or humidifier to keep the air moist. Gently applying a thin layer of petroleum jelly just inside the nostrils can also help lock in moisture — but only with clean hands and in moderation.
2. Watch Out for Nose Picking or Frequent Blowing
We get it — sometimes, blowing the nose brings relief. But repetitive picking or aggressive nose-blowing can irritate and rupture tiny blood vessels in the nose, especially in older adults with thinner skin and weaker blood vessels.
Prevention Tip: Encourage gentle nose hygiene, offer tissues instead of handkerchiefs, and consider talking to a GP if dry crusting or frequent blockages are common (they may suggest saline rinses or medicated ointments).
3. Avoid Overuse of Nasal Sprays
Some over-the-counter decongestants (like oxymetazoline) can dry out the nasal lining when used too often, actually increasing the risk of nosebleeds. According to Griswold Home Care, overuse is a sneaky but common cause in seniors managing sinus pressure or allergies.
Prevention Tip: Stick to the “three-day rule” for decongestants, and talk to a GP about safer long-term alternatives if nasal congestion is a recurring issue.
4. Manage Underlying Health Conditions
High blood pressure, blood thinning medications, and certain chronic conditions like liver disease or clotting disorders can all raise the risk of spontaneous nosebleeds. Regular monitoring and check-ins with a doctor are essential, especially if nosebleeds are frequent or hard to stop.
Prevention Tip: If your loved one is on warfarin or aspirin, be proactive about their INR checks or clotting profiles. Let their GP know about any new or worsening bleeding episodes.
5. Stay Hydrated
It’s simple, but powerful — staying hydrated supports skin elasticity, keeps mucous membranes moist, and helps regulate blood pressure. Dehydration, especially in warm weather or due to certain medications (like diuretics), can dry out the nose from the inside out.
Prevention Tip: Offer sips of water throughout the day and monitor fluid intake in those with memory concerns or swallowing difficulties. Adding hydrating foods like cucumber, watermelon, and soups can also help.
Caring Through Preparedness
Nosebleeds in older adults can be unsettling — not just for the person experiencing them, but for the carers and family members supporting them. But here’s the good news: when you understand the causes, take a few preventative steps, and know how to respond confidently, nosebleeds stop being scary and start being manageable.
Whether you’re caring for a loved one at home, supporting clients in residential care, or simply looking for better ways to prepare, your role matters. Compassion and calm go a long way — and having the right tools on hand makes all the difference.
At Platinum Health Supply, we’re here to make your job easier, safer, and more informed. From first aid essentials to specialised care products like Rapid Rhino Nasal Tamponade Devices, medical-grade gloves, and ergonomic lift chairs, we’ve got your back.
Visit Our Epping Showroom!
Prefer to see products in person or chat with someone about your care needs?
Come say hi at:
Unit 2/51 Trafalgar Road, Epping VIC 3076
Monday to Friday, 9:00 AM – 5:00 PM
Our friendly team can walk you through wound care, aged care, and emergency response essentials — no pressure, just helpful advice.
Not Local? No Worries.
You can also browse our full range online and enjoy fast, Australia-wide delivery.
You're doing a brilliant job. We're here to support you, one care moment at a time.
Important Disclaimer
This blog is intended for informational and educational purposes only. It draws upon publicly available health resources and best-practice guidelines to support carers and families — but it is not a substitute for professional medical advice, diagnosis, or treatment.
If you or someone you care for is experiencing frequent, severe, or unexplained nosebleeds, please consult a qualified healthcare provider. Any medical products mentioned (such as nasal tamponades or lift chairs) should only be used as directed and may not be suitable for everyone.
Platinum Health Supply Group is a healthcare supplies provider, not a medical clinic. We do not assume liability for outcomes resulting from the application of information in this blog without appropriate medical consultation.
When in doubt, always check with a GP, nurse, or emergency services — especially if a situation feels urgent or out of the ordinary.
