How to Help Someone Gain Weight Safely in Aged Care

You might find yourself wondering:
Are they eating enough?
Is it the medication?
Do they just not like the food?
The truth is, unintentional weight loss in older adults is more than just a numbers game on the scale. It can lead to muscle loss, fatigue, lower immunity, and even a greater risk of falls or hospital stays.
But here’s the good news: with the right approach, it is possible to help someone regain strength, energy, and confidence — one meal, one snack, and one small win at a time.
We’ll walk you through realistic, kind strategies to help someone gain weight safely in aged care. No pressure. No shame. Just practical, person-first care rooted in empathy and nourishment.
What Causes Weight Loss in Older Adults?
When someone in aged care starts to lose weight, it’s rarely just about smaller portions or skipped meals. There’s usually more going on beneath the surface. In fact, unintentional weight loss in seniors is often caused by a combination of physical, emotional, and even environmental factors.
Here’s what might be at play — and why it’s important to look beyond the dinner plate.
1. Medical Conditions and Chronic Illness
Many health issues common in older adults can affect appetite, digestion, or metabolism. According to the American Family Physician Journal and the Mayo Clinic, underlying conditions like cancer, chronic infections, thyroid disorders, gastrointestinal diseases, or even heart failure can all contribute to unintentional weight loss.
Sometimes, the weight loss is one of the first signs something’s not right — which is why it should never be brushed off.
2. Medication Side Effects
Ever noticed a drop in appetite after starting a new medication? You're not imagining it. Medications like antidepressants, diuretics, and certain painkillers can cause nausea, change taste perception, or reduce hunger altogether. According to Stellis Health and research in the Canadian Medical Association Journal, polypharmacy (taking multiple medications at once) is a frequent culprit in appetite loss among seniors.
3. Mental Health & Cognitive Changes
Depression, anxiety, and grief are powerful factors that can suppress appetite. For individuals living with dementia or Alzheimer’s, forgetting to eat — or forgetting how to eat — is also common. CareHop highlights emotional wellbeing as a key factor, noting that loneliness or isolation can significantly impact motivation around meals.
4. Dental or Swallowing Issues
Chewing and swallowing might not seem like big deals — until they are. Ill-fitting dentures, sore gums, dry mouth, or dysphagia (swallowing difficulties) can all make eating uncomfortable or even painful. When eating becomes a chore, it's no wonder food starts to lose its appeal.
One helpful support option is Gloup Medication Lubricant. It's a swallowing gel that helps make medications easier to take — especially for those who struggle with dry mouth or find pills difficult to swallow.

While Gloup is often used for meds, it can also help reduce the stress of swallowing in general, which might encourage better food intake in some situations. If you're not ready to commit to a big bottle, Gloup is also available in 150ml.
Important: If swallowing issues are present, always consult a GP, speech pathologist, or your loved one’s care team before making changes to meals or introducing any swallowing aids. They can help assess the underlying cause and recommend safe strategies based on individual needs.
5. Sensory Changes (Taste and Smell)
As we age, our senses naturally dull — especially taste and smell. This makes food seem bland or unappealing, leading to smaller portions or skipped meals. According to CareHop and Mayo Clinic, these subtle changes often go unnoticed, but they can have a major impact on food enjoyment and intake.
6. Limited Mobility or Physical Fatigue
Even preparing a meal or sitting up for long periods can be physically draining for some older adults. If the effort to eat outweighs the energy they have to give, meals may get skipped altogether. In institutional or home care settings, fatigue or illness-related weakness can also interfere with regular feeding routines.
Simple Nutrition Strategies for Healthy Weight in Aged Care
Once you've ruled out or managed any underlying causes of weight loss, the next step is all about nourishing meals — the kind that are energy-dense, nutrient-rich, and still a joy to eat.
For older adults, it’s not just about piling on calories — it's about making every bite count. According to Nutrition Australia and the National Institute on Aging, meals should focus on balance, variety, and ease of eating, especially when appetite is low.
Think: soft textures, warm flavours, and smaller portions served more frequently throughout the day.
Here are a few practical ways to help:
1. Prioritise Energy-Dense, Nutrient-Rich Foods
Instead of large portions, think small but mighty. Focus on meals and snacks packed with protein, healthy fats, and essential vitamins.
According to Nutrition Australia, simple tweaks like using full-cream milk, adding avocado or cheese to meals, or drizzling olive oil over veggies can boost nutrition without overwhelming the appetite.
Try this: Fortisip Compact Protein
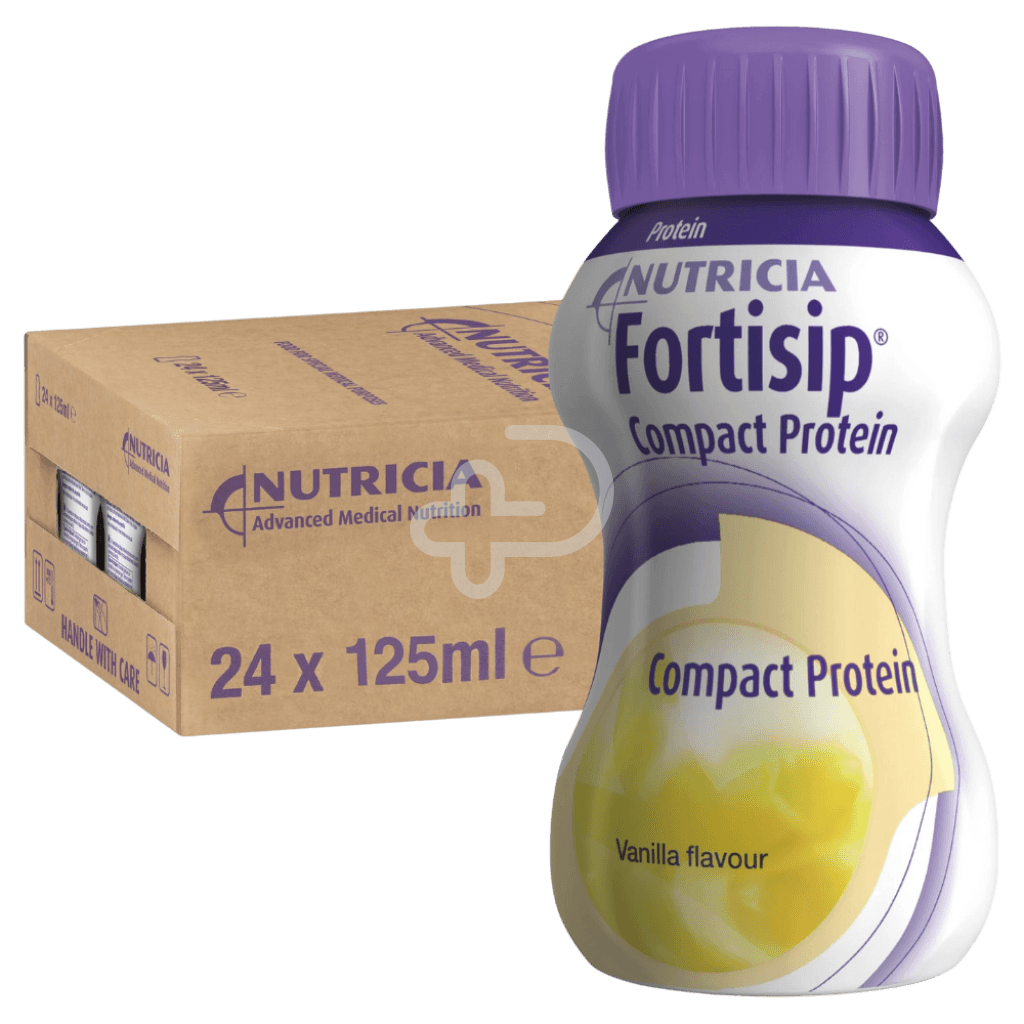
This compact, high-protein drink packs serious nutrition into a small serving — ideal for older adults with reduced appetite. Easy to drink, easy to digest, and available in a range of flavours.
2. Add in Nourishing Between-Meal Snacks
Not everyone feels up to three full meals a day — but gentle snacking can make all the difference. The National Institute on Aging recommends nutrient-rich snacks like yoghurt, cheese, nut butters, and oral nutrition beverages to boost daily intake.
Try this: Nestlé Resource Ultra Clear

This refreshing fruit-flavoured drink delivers high-quality whey protein isolate along with essential vitamins — perfect for topping up energy between meals or when taste fatigue kicks in.
3. Make Mealtimes Enjoyable
People eat more when they feel relaxed and engaged. A warm, social environment can do wonders — even just playing soft music or sitting down together can improve appetite.
As bpacnz highlights, mealtime routines also help establish a sense of normalcy, dignity, and comfort in aged care.
4. Address Texture and Swallowing Challenges
Soft, smooth foods are essential for older adults with chewing or swallowing issues. Scrambled eggs, stewed fruits, mashed vegetables, or custards are all gentle choices.
For those on enteral nutrition, tube feeding formulas are key to ensuring complete and balanced intake.
Try this: Nutrison Protein Plus

Formulated for patients using a feeding tube, this high-protein formula supports weight gain and maintenance in older adults who can’t meet their needs through oral intake alone.
5. Keep Hydration Front and Centre
Even mild dehydration can worsen fatigue and loss of appetite — but older adults often drink less. Water, tea, milk, and juice all count.
Tip: Offer meals in a calm, unhurried setting. Support autonomy by allowing your loved one to choose what and when they eat — and remember, every small win counts.
What to Watch For (and When to Get Help)
Weight loss in older adults doesn’t usually happen overnight — and sometimes, the signs can be easy to miss until it’s already taken a toll. That’s why it’s so important for carers and family members to stay observant, curious, and proactive.
Here are some of the most common red flags to keep an eye on:
1. A Sudden Drop in Appetite
A consistently untouched plate or a polite “I’m not hungry” at every mealtime isn’t just about being picky — it could be an early sign of something deeper. According to A Place for Mom, appetite loss in the elderly can stem from both physical conditions (like pain or medication side effects) and emotional ones (like depression or loneliness).
What you can do:
- Gently encourage smaller, frequent meals
- Introduce favourite foods or comforting smells
- Consider consulting a GP or dietitian if the appetite loss continues for more than a few days
2. Noticeable Weight Loss (Clothes Fitting Looser, Belts Tighter)
You may not always have access to a scale, but your eyes and instincts are just as powerful. Clothes that suddenly hang off the body, jewellery slipping off, or visible collarbones where there weren’t before — these are all signs to investigate.
Tip: Start a simple log — jot down daily meals, snacks, and any missed meals. It helps identify patterns and provides a clear picture if you need to speak to a healthcare provider.
3. Withdrawing from Mealtimes
According to Stellar Care, elderly individuals may start avoiding the dinner table altogether due to embarrassment (from struggling to chew or use cutlery) or simply because they feel disinterested in food.
This can be especially common in those living with dementia or cognitive decline. The Alzheimer’s Society notes that sensory changes, confusion, or difficulty recognising food can all contribute to mealtime stress.
What you can do:
- Offer finger foods or easy-to-eat options
- Reduce distractions during mealtimes
- Make mealtimes a calm, reassuring experience — not a battleground
4. Digestive Discomfort or Fatigue After Meals
If someone starts avoiding food because they feel bloated, nauseous, or sleepy afterward, it may indicate issues with digestion or the type of food being offered.
What you can do:
- Offer smaller meals more often
- Avoid heavy, greasy foods
- Ensure hydration levels are adequate
Don’t forget — nutrition is about comfort as much as it is about calories.
When to Reach Out
If your loved one…
- Is losing weight rapidly
- Consistently refuses food or drink
- Shows signs of dehydration
- Seems confused or fatigued after meals
- Has difficulty swallowing (dysphagia)
…it’s time to speak to a GP, dietitian, or care team.
Early support can make a big difference in preventing complications like malnutrition, pressure sores, or hospital admissions.
Let’s Nourish with Care
Helping an older adult gain weight safely isn’t just about calories — it’s about restoring confidence, comfort, and quality of life. Whether it’s tweaking meals, introducing supplements, or finding new ways to make food enjoyable again, every small action adds up to something meaningful.
If you’re a carer, family member, or aged care professional navigating this journey, know this: your care matters. And you don’t have to figure it all out by yourself.
At Platinum Health Supply, we’re here to support you with more than just products. Our team understands the daily challenges of home care — and we’re always ready to help you choose the right nutritional support, feeding aids, or home care essentials tailored to your loved one’s needs.
Visit our Epping Showroom at Unit 2/51 Trafalgar Road, Epping VIC 3076
We’re open Monday to Friday, 9 AM – 5 PM
Whether you’re after oral nutrition supplements, feeding solutions, or just some friendly advice — pop in for a chat. You’ll find a welcoming space, a knowledgeable team, and solutions that truly support your care journey.
Not nearby? Explore our full oral nutrition range online with fast, Australia-wide delivery.
Because every older adult deserves to feel strong, supported, and well-nourished — and every carer deserves a little backup.
Important Disclaimer
This blog is intended for informational purposes only. While we do our best to reference publicly available health information and expert-backed resources, it is not a substitute for professional medical advice, diagnosis, or treatment.
Before introducing any new nutritional products, supplements, or feeding solutions to an older adult — especially those with existing health conditions — always consult with a doctor, dietitian, or qualified healthcare provider. What works well for one person may not be suitable for another.
Platinum Health Supply Group provides healthcare products, not clinical care. We are not a hospital, clinic, or medical authority, and we cannot be held responsible for outcomes resulting from the use or misuse of information provided in this blog without medical consultation.
