How to Monitor Wounds Without Removing the Dressing

Wound care is a balancing act — you want to make sure everything’s healing well, but checking too often can do more harm than good. Removing a dressing just to “take a quick look” can lead to delayed healing, discomfort, and increased infection risk — especially in aged care or home settings where skin may already be fragile.
Thankfully, there are safer, smarter ways to monitor wounds without disturbing them. With a bit of know-how and the right products, you can track healing progress without lifting the dressing every time.
In this guide, we’ll walk you through how to observe wounds safely, what signs to look out for, and which dressings make monitoring easier for both carers and clinicians.
Why Frequent Dressing Changes Can Cause More Harm Than Good
It’s natural to want to check on a wound often — especially when you’re caring for someone at home or in aged care. But more frequent isn’t always better. In fact, constantly removing and replacing dressings can actually slow healing, increase discomfort, and elevate the risk of infection.
1. It Disturbs the Healing Environment
According to Wounds International, wounds heal best in a moist, undisturbed environment. Every time a dressing is removed, the wound is exposed to air, bacteria, and potential trauma — essentially resetting the healing process.
This is especially important for chronic wounds or fragile skin conditions, where the risk of tissue damage is already high.
2. It Increases Pain and Skin Trauma
For older adults or people with sensitive skin, dressing removal isn’t just an inconvenience — it can be painful. The act of lifting an adhesive or disturbing a semi-healed wound can re-damage new tissue, leading to delays and added distress.
As outlined by the Wound Care Education Institute, excessive dressing changes may also lead to skin stripping, irritation, and unnecessary exposure to adhesives or cleaning solutions — especially problematic in aged care or disability settings.
3. It Wastes Supplies (and Time)
Frequent changes also mean higher use of gloves, cleansing agents, tapes, and dressing materials. This not only drives up costs but also creates more waste — and can lead to carer burnout when changes feel endless and unnecessary.
As noted in a clinical overview by the NCBI, optimal wound care involves choosing dressings that support longer wear times and minimise the need for disruption — especially in environments where healthcare resources or trained staff may be limited.
The Key Takeaway?
Less is often more. With the right dressing in place and a smart monitoring approach, you can give the wound the stability it needs to heal — while still keeping a close eye on progress.
How to Monitor Wounds Without Removing the Dressing
Monitoring a wound is essential — but doing it without peeling back the dressing requires a bit of insight, some modern tools, and a good dose of trust in the healing process. The goal is to catch early signs of trouble without disrupting the progress that’s already happening under the surface.
Here’s how carers and clinicians can assess wounds safely and effectively — without removing the dressing every time.
1. Watch for External Clues
Before reaching for the tape, take a moment to assess the area around the dressing. According to The Royal Children’s Hospital wound care guidelines, these are some of the most telling signs you can observe from the outside:
- Increased leakage or strike-through on the dressing
- Change in odour
- Redness or warmth around the wound margins
- Swelling or visible inflammation
- Pain or discomfort reported by the patient
Any of these may indicate that it’s time to safely inspect or change the dressing — but without these flags, it’s often best to leave it undisturbed.
2. Use Smart Dressings
One of the easiest ways to reduce dressing changes is to use technology that does the monitoring for you — and negative pressure wound therapy (NPWT) is a game-changer in this space.
The PICO 7 Single Use Negative Pressure Wound Therapy System offers a portable, low-maintenance solution for managing a wide range of wound types, from surgical incisions to ulcers and partial thickness burns. What makes it particularly useful for carers and clinicians? It includes a dressing change indicator, so you’ll know exactly when it’s time to intervene — no guesswork required.
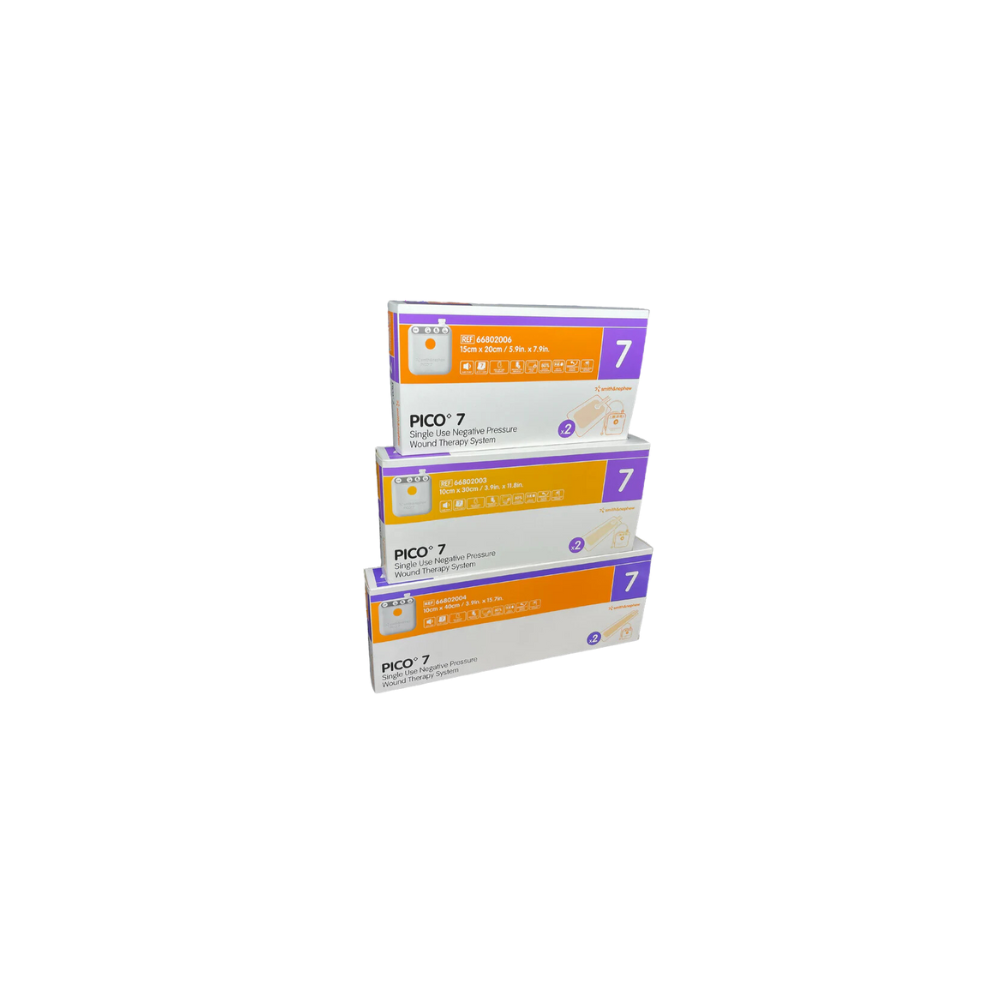
According to Wounds UK, systems like PICO support longer dressing wear times (up to 7 days), better fluid management, and consistent wound pressure — which all contribute to faster healing with fewer disruptions. Plus, the PICO 7’s compact, wearable design means it’s suited for both hospital and home care settings, making wound care more comfortable and mobile-friendly for the person you're supporting.
Bonus: Its start-date tracker and AIRLOCK Technology make it easier to assess healing progress externally — while maintaining a closed, protected wound environment.
3. Know What’s Normal — and What’s Not
Knowing the baseline appearance and behaviour of a wound helps you recognise when something’s changing. Spectral AI recommends recording wound details at the start of treatment (even a simple photo and chart) to track progression. This way, you can make observations like:
- Is the dressing staying dry, or becoming more saturated over time?
- Is there increased odour or warmth?
- Is the patient showing signs of new discomfort or sensitivity?
Monitoring doesn't have to be invasive — but it does need to be consistent.
4. Use the TIME Framework (Without Lifting the Dressing)
The TIME acronym — Tissue, Inflammation/Infection, Moisture balance, Edge of wound — is a recognised tool in wound assessment. While you can’t always see inside, you can infer many of these factors from dressing condition and patient feedback.

T = Tissue (What’s Going on Underneath?)
Healthy tissue is usually pink or red and moist — but necrotic (dead) or sloughy tissue can slow healing.
What to look/listen for:
- Has the dressing stayed in place without leakage?
- Is the person reporting less pain or discomfort?
- Is the wound odour improving, staying neutral, or worsening?
If you’re using a transparent or semi-occlusive dressing, you might even be able to visualise tissue colour or slough formation without removal.
I = Inflammation or Infection
Some inflammation is normal — but excessive heat, pain, swelling, or odour may point to infection.
What to watch for:
- Dressing appears swollen or leaking with discoloured fluid
- Strong or unpleasant smell through the dressing
- Redness or warmth in surrounding skin
- A sudden increase in reported pain
These could all be signs that the wound is infected or not progressing as expected.
M = Moisture Balance
Moisture is crucial for healing — too much and you risk maceration; too little and the wound dries out and slows down.
What to monitor:
- Does the dressing look soggy or saturated (strike-through)?
- Is the adhesive lifting from excess fluid?
- Is the person experiencing itchiness or discomfort around the site?
Some advanced dressings like hydrocolloids or NPWT systems (like PICO 7) have built-in indicators that show when moisture levels are off — a huge help in real-time monitoring.
E = Edge of Wound
Healthy wound edges should appear even and show signs of epithelialisation (skin regrowth). Rolled or irregular edges could indicate stalled healing.
What to check for:
- Are there signs of redness or damage around the dressing borders?
- Any spreading rash, irritation, or tightness around the wound edges?
- Does the person say it feels tighter or more painful than before?
If the dressing is bulging, lifting, or puckering, it might be a sign the wound is no longer responding well — and needs reassessment.
As highlighted in ScienceDirect’s review on advanced wound assessment and the NCBI wound care guidelines, using structured frameworks like TIME helps guide wound care decisions even when visibility is limited.
5. Final Tip: Trust the Dressing — and Document What You See
According to the Wound Care Alliance UK, dressings are designed to stay in place for 3–7 days depending on the wound type and environment. If there’s no visible concern, let the dressing do its job.
Keep a simple log of:
- Dressing condition (dry, moist, odorous)
- Any changes in skin around the site
- Pain levels or behavioural cues
- Time since last change
Documentation + smart dressing choices = better outcomes without disruption.
Products That Support Healing Without Frequent Dressing Changes
When you're trying to monitor a wound without disturbing the dressing, the key is choosing products designed to do the hard work for you — whether through smart visual indicators, extended wear times, or gentle removal technologies. Here are a few trusted options we recommend for carers and clinicians alike:
1. Mepilex Border Flex Lite

Order the Mepilex Border Flex Lite Now!
Flexible, Low-Profile Coverage for Fragile Skin
This ultra-conformable dressing is ideal for non- to moderately exuding wounds such as pressure ulcers, surgical wounds, and skin tears. The built-in Safetac® layer ensures pain-free removal, while the breathable waterproof backing helps you monitor for leakage or strike-through without removal.
Why it’s perfect for low-disturbance monitoring:
- Visual cues for exudate build-up
- Extended wear time with gentle adhesion
- Protects fragile skin while supporting healing
2. Molnlycke Mepilex Silver Foam Dressing

Order the Molnlycke Mepilex Silver Foam Dressing Now!
Advanced Healing for At-Risk or Infected Wounds
This antimicrobial dressing combines silver ion technology with high fluid-handling capacity, making it a go-to for wounds that are at risk of infection or not progressing well. The soft, flexible design contours to tricky areas like elbows or heels, and the Safetac® layer allows for low-pain removal — meaning you can monitor and manage without disruption.
Why it’s great for wound monitoring:
- Can stay in place for up to 7 days
- Visual signs of saturation help guide change timing
- Reduces bacterial load to support faster healing
3. Molnlycke Mepitel Wound Contact Dressing

Order the Molnlycke Mepitel Wound Contact Dressing Now!
The Gentle Middle Layer That Lets You Check Without Disturbing the Wound
Mepitel is a transparent, non-absorbent wound contact layer with an open mesh structure that lets exudate pass through to a secondary dressing. This means you can change the outer layer without touching the wound bed — ideal for delicate wounds like skin tears, grafts, or diabetic ulcers.
Why it helps with wound visibility:
- Transparent mesh lets you view the wound through the dressing
- Reduces need to disturb healing tissue
- Minimises trauma during dressing changes
Also Helpful: Skin-Friendly Barrier Protection & Moisturisers
Sometimes it’s not just the wound you need to care for — it’s the surrounding skin, especially when dealing with moisture, adhesives, or frequent contact.
4. 3M Cavilon No Sting Barrier Film Spray

Order the 3M Cavilon Barrier Film Spray Now!
A protective spray that shields skin from friction, adhesives, and moisture
If dressings or wound exudate are irritating the skin around the wound, this alcohol-free barrier film provides invisible protection without stinging — ideal for aged care, incontinence-related skin issues, or wounds near joints.
5. Molnlycke Epaderm Cream

Order the Molnlycke Epaderm Cream Now!
For dry, eczema-prone, or sensitive skin surrounding the wound site
A gentle, fragrance-free emollient that’s perfect for keeping periwound skin hydrated and protected — especially when dryness or flaking may compromise dressing adhesion or comfort.
Less Disturbance, Better Healing
Wound care doesn't have to be a daily guessing game — and it definitely shouldn't cause more harm than good. By choosing the right products and using smart assessment techniques, you can confidently monitor wound progress without disrupting healing or adding unnecessary stress to the person you're supporting.
Whether you're a clinician, carer, or family member, remember: healing is a team effort, and with the right tools, it's possible to make every step gentler, safer, and more effective.
Need Wound Care Supplies You Can Trust?
Come visit us at our Epping showroom — our friendly team can walk you through the best wound dressings, barrier creams, and advanced therapies to suit your needs.
Platinum Health Supply Group
Unit 2/51 Trafalgar Road, Epping VIC 3076
Monday to Friday | 9:00 AM – 5:00 PM
Prefer to shop from home? Browse our full wound care range online with fast, Australia-wide delivery and expert-backed product options to help make wound care easier — and healing more comfortable.
Because less disruption means more healing. Let’s support better outcomes, together.
Important Disclaimer
This blog is intended for informational and educational purposes only and is based on publicly available wound care guidelines and best-practice resources.
Platinum Health Supply Group is not a medical provider, and this content should not be used as a substitute for professional medical advice, diagnosis, or treatment.
Wounds — especially those that are slow to heal, infected, or related to chronic conditions — require proper clinical assessment. If you're unsure about a wound's condition, notice signs of infection, or are considering new dressings or therapy systems, please consult a doctor, nurse, or wound care specialist before making changes.
Always follow your healthcare provider’s instructions and care plan. Your healthcare team is your best resource for ensuring safe, effective wound management.
