When is a Nosebleed a Medical Emergency? A Practical Guide for Carers and Families

If you’re a carer, support worker, or family member looking after someone vulnerable, knowing the difference between a harmless nosebleed and a potential emergency is crucial. It’s not about jumping to worst-case scenarios — it’s about having the confidence to act calmly, quickly, and safely when it matters.
In this guide, we’ll walk you through how to manage a nosebleed, what to do when a nosebleed won’t stop, and when to seek urgent help — especially if you’re supporting NDIS participants, elderly loved ones, or people with health conditions.
What Causes Nosebleeds in Elderly and Vulnerable People?
Nosebleeds can happen to anyone, but they’re often more frequent, longer-lasting, or harder to manage in elderly people or those with certain medical conditions.
According to Ambulance Victoria, nosebleeds (technically known as epistaxis) are usually caused by broken blood vessels inside the nose — often from dryness, irritation, or injury. But in older adults or people with health issues, there may be other reasons to watch for.
Here are some of the most common causes in elderly or vulnerable individuals:
1. Fragile Blood Vessels
As we age, the blood vessels inside the nose can become thinner and more delicate. Even minor irritation — like blowing the nose or dry air — can cause them to break.
2. Medications That Affect Bleeding
Blood thinners (like warfarin, aspirin, or clopidogrel) can make a small nosebleed much harder to stop. Some people may also bruise or bleed more easily if they’re on long-term anti-inflammatory medications.
3. Dry Air or Oxygen Therapy
Indoor heating, air conditioning, and medical oxygen can all dry out the lining of the nose — especially in winter or aged care settings — making it more prone to cracking and bleeding.
4. Nose-Picking or Rubbing
Yes, it happens more often than you think — especially in people with dementia, cognitive conditions, or sensory needs who may not realise they’re doing it.
5. Underlying Health Conditions
According to the Mayo Clinic, people with high blood pressure, liver disease, bleeding disorders, or autoimmune conditions may be more likely to experience severe or persistent nosebleeds.
6. Unknown or Spontaneous Causes
Sometimes, a nosebleed seems to come out of nowhere — and that’s okay. But if they’re frequent, unexplained, or hard to stop, it’s worth checking in with a GP to rule out anything serious.
As University Hospitals explains, nosebleeds in older adults should always be taken seriously if they’re accompanied by dizziness, confusion, or other signs of distress.
How to Tell If a Nosebleed Is a Medical Emergency
Most nosebleeds look dramatic, but they’re usually nothing to panic about. That said, some situations absolutely call for medical attention — especially when you're caring for someone elderly, unwell, or prone to complications.
Here’s how to tell the difference between a common nosebleed and one that needs professional care.
Signs a Nosebleed Is a Medical Emergency
According to Better Health Victoria and the Mayo Clinic, you should call Triple Zero (000) or go to hospital if:
- The bleeding doesn’t stop after 20 minutes, even with pressure applied
- The person is dizzy, weak, confused, or fainting
- The nosebleed follows a fall, head injury, or blow to the face
- There’s a lot of blood, or it’s running down the throat and causing choking
- The person is vomiting blood or coughing up blood-stained mucus
- You see bleeding from both nostrils at once, which can be a sign of deeper trauma
- The person is on blood-thinning medication or has a bleeding disorder
Additional Red Flags in Elderly or Vulnerable People:
- The person is already frail, unsteady, or recovering from illness
- They’re unable to follow instructions to pinch the nose or lean forward
- They’re using oxygen or have medical tubing that could complicate airway safety
- You notice repeated nosebleeds with no clear cause
As the American College of Emergency Physicians puts it: if the nosebleed is causing distress, feels out of control, or puts the person at risk of breathing or circulation issues, it’s time to get help.
What Might Happen at the Hospital?
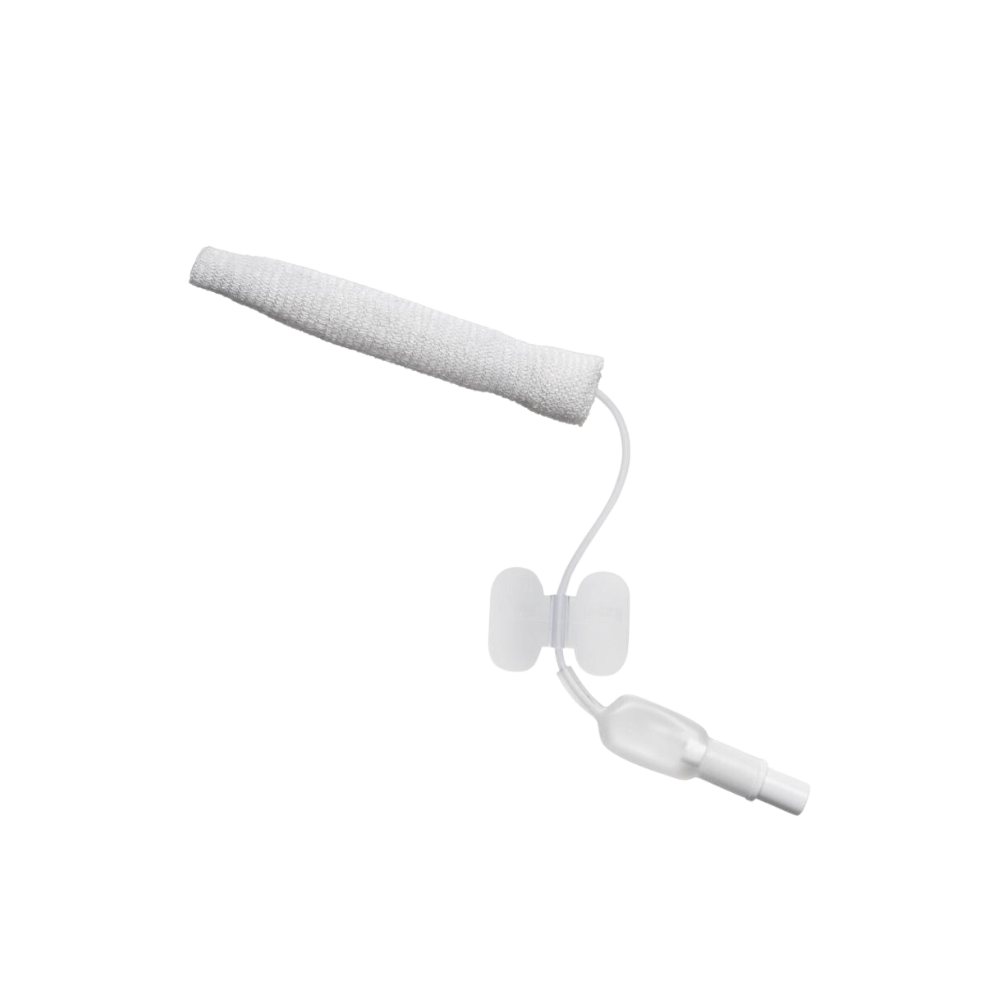
In some cases, the hospital team may use a nasal tampon device like Rapid Rhino — a soft, expandable product that helps stop bleeding fast by applying direct pressure inside the nose. It’s designed for more serious nosebleeds that don’t respond to first aid.
It’s always better to act early than wait too long. If you’re not sure — call your GP, local urgent care service, or Healthdirect Australia on 1800 022 222 for 24/7 advice.
First Aid for Nosebleeds: What to Do (and What Not to Do)
If you’re caring for someone and their nose suddenly starts bleeding, it can look alarming — especially if they’re older or have other health conditions. But with a calm approach and a few simple steps, most nosebleeds can be managed safely at home.
Here’s a step-by-step guide to first aid for a nosebleed, based on recommendations from Better Health Victoria and Mayo Clinic.
What to Do:

1. Stay calm and reassure the person
Panicking can make bleeding worse. Keep the person seated and relaxed.
2. Have them lean forward slightly
This stops blood from running down the throat, which can cause choking or nausea.
3. Pinch the soft part of the nose (not the bridge)
Use your thumb and index finger to gently pinch the nostrils closed. Maintain steady pressure for at least 10 minutes — use a timer.
4. Use a tissue or cloth to catch any drips
Encourage them to breathe through their mouth and avoid sniffing or blowing their nose.
5. Apply a cool compress to the back of the neck or forehead (optional)
This may help slow bleeding, but it’s not essential.
What Not to Do:

- Don’t lean the person back — it may cause blood to run down the throat.
- Don’t pack the nose with tissues, cotton balls, or paper — these can cause irritation and worsen bleeding.
- Don’t check too early — releasing pressure before the full 10 minutes can restart bleeding.
- Don’t give aspirin or anti-inflammatories unless advised by a doctor — they can thin the blood.
If It Doesn’t Stop...
If the bleeding hasn’t slowed or stopped after 20 minutes, or if the person becomes faint, confused, or distressed, seek medical help immediately. Hospitals may use specialised products like Rapid Rhino — a nasal tampon designed to stop bleeding quickly and safely in emergency settings.
Remember: If you’re not sure whether to keep managing it or escalate, call Healthdirect Australia on 1800 022 222 or go straight to the nearest urgent care service.
Helpful Products for Managing Nosebleeds with Confidence
Whether you're caring for someone at home, in aged care, or on the move, having the right supplies nearby can make all the difference when a nosebleed happens. Here are a few trusted products that can support both everyday care and more serious situations.
1. Rapid Rhino Inflatable Tamponade Device
When a nosebleed won’t stop, hospital teams may turn to Rapid Rhino — a specially designed inflatable nasal tamponade device that applies gentle, targeted pressure inside the nasal cavity to stop bleeding fast.
While not a home-use item, it’s helpful for carers and families to know what may be used in emergency care or aged care settings. Some clinical providers may also stock Rapid Rhino as part of their emergency treatment protocol for severe epistaxis.
Best for:
Hospitals, aged care facilities, clinical settings with trained staff.
2. Voyager 2 Series Plastic Neat First Aid Kit

This compact first aid kit is ideal for carers, support workers, and families who want to stay prepared — whether at home, on the road, or at a community event. It includes wound pads, gloves, wipes, and basic care items to safely manage minor bleeding events like nosebleeds.
Why it's useful:
- Keeps essentials in one easy-to-access case
- Portable and workplace-compliant
- Great for personal or professional use
Best for:
Home care, support workers, day programs, or mobile staff needing ready access to basic first aid.
3. Combine Dressing Roll – Non-Woven

This soft, absorbent dressing roll is perfect for gently catching blood drips or wiping around the nose without causing further irritation. It can be cut to size and is non-woven, making it a skin-friendly option during or after a bleed.
Why it helps:
- Gentle on delicate or elderly skin
- Absorbs blood without sticking to the skin
- Easy to store in kits or care bags
Best for:
At-home care, support workers, and aged care environments managing frequent or minor nosebleeds.
Know What to Do, and When to Act
Most nosebleeds are nothing to worry about — but when you’re caring for someone vulnerable, it helps to know exactly what to do and when it’s time to call for help. A few simple first aid steps, a calm approach, and the right supplies can go a long way in keeping things under control.
And if a nosebleed won’t stop? You now know what to look for, how to respond, and that tools like Rapid Rhino may be used in clinical settings to get things under control fast.
Whether you’re a family carer, aged care worker, or NDIS support provider, having the right first aid essentials close by gives you peace of mind — and practical confidence when it counts.
Need to stock up on nosebleed care supplies? Browse our range of first aid kits and absorbent dressings.
📍 Prefer to speak to someone in person?
Visit our Epping store at Unit 2/51 Trafalgar Road, Epping VIC 3076
Open Monday to Friday, 9:00 AM – 5:00 PM
We’re here to help you care with confidence — because being prepared isn’t just for emergencies. It’s part of everyday support.
Important Disclaimer
Platinum Health Supply Group is a healthcare supplies provider, not a hospital, clinic, or emergency medical service. This blog is intended for general informational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment.
If you or someone in your care is experiencing a severe or persistent nosebleed, or you are ever unsure about what to do, please seek immediate medical attention or call Triple Zero (000) in an emergency.
For personalised medical advice, speak to a GP, emergency doctor, or healthcare professional.
We share this information to help carers, families, and support workers feel more prepared — but clinical decisions should always be made by trained professionals.